In the annals of public health history, pivotal moments have often been marked by the release of influential reports that have shaped the trajectory of societal attitudes and behaviors.
Sixty years ago, the U.S. surgeon general released a landmark report that definitively settled a longstanding public debate about the dangers of cigarettes, ultimately leading to transformative changes in smoking habits across America.
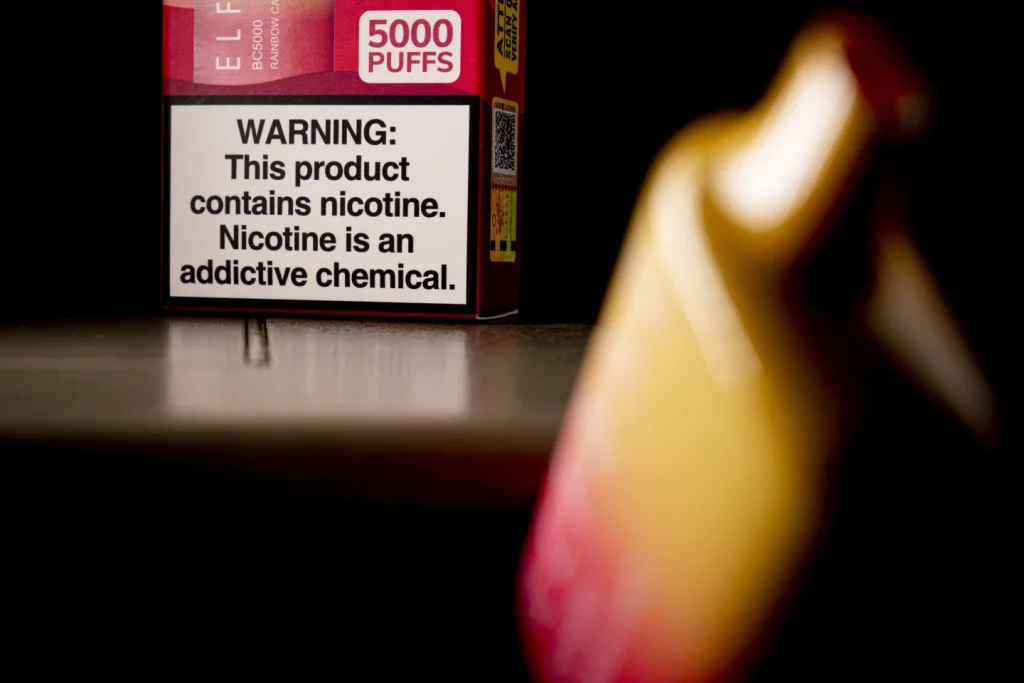
Today, as the public grapples with the rise of vaping, there is a growing call for a similar clarifying report to address the myriad of uncertainties surrounding electronic cigarettes.
The debate has intensified as conflicting messages about the relative risks of vaping compared to traditional cigarette smoking have left the public and policymakers uncertain about the true dangers and benefits of e-cigarettes.
This essay seeks to explore the urgent need for clarity on the topic of vaping, examining the current state of knowledge, the challenges posed by the lack of long-term evidence, and the potential impact of a surgeon general’s report on public perceptions and policy decisions.
In the contemporary landscape, there exists a pervasive misconception among U.S. adults that nicotine vaping is as harmful as, or even more dangerous than, cigarette smoking.
This misconception has been fueled by a complex web of conflicting information and mixed messages, leading to widespread confusion and uncertainty.
Despite the consensus among the U.S. Food and Drug Administration and the majority of scientists that electronic cigarettes are indeed less dangerous than traditional cigarettes, a cloud of ambiguity continues to shroud the public discourse on vaping.
Lawrence Gostin, a distinguished public health law expert at Georgetown University, emphasizes the urgent need for clarity, asserting that a surgeon general’s report could effectively dispel the prevailing confusion and misconceptions surrounding vaping.
While it is essential to acknowledge that e-cigarettes are less harmful than traditional cigarettes, it is equally imperative to recognize that they are not entirely harmless.
The potential risks and benefits of vaping remain a subject of heated debate among public health experts, underscoring the critical need for comprehensive, evidence-based information to guide public understanding and policy formulation.
Dr. Kelly Henning, who leads the public health program at Bloomberg Philanthropies, highlights the remarkable lack of evidence due to the relatively short duration of e-cigarettes in the market.
This lack of long-term evidence poses a significant obstacle in accurately assessing the potential health impacts of vaping, particularly in relation to the development of serious conditions such as lung cancer and heart disease.
The absence of long-term data on the health effects of vaping presents a formidable challenge in evaluating the true risks and benefits associated with electronic cigarettes.
Traditional epidemiological studies, which rely on extended periods of observation to detect the emergence of health outcomes, are essential in ascertaining the long-term impacts of any given behavior or exposure.
However, the relatively recent emergence of e-cigarettes has precluded the availability of robust longitudinal data, thereby hindering the ability of scientists and public health experts to make definitive conclusions about the potential health consequences of vaping.
This critical knowledge gap has contributed to the prevailing uncertainty and conflicting messages surrounding the safety and efficacy of e-cigarettes, further underscoring the pressing need for a comprehensive assessment of the available evidence.
A surgeon general’s report on vaping has the potential to catalyze a paradigm shift in public perceptions and policy decisions.
By consolidating and synthesizing the existing scientific evidence, such a report could serve as a definitive resource to dispel misconceptions and provide clear guidance on the relative risks and benefits of vaping.
Furthermore, a surgeon general’s report has the power to influence public health policies, regulatory frameworks, and educational initiatives, ultimately shaping the trajectory of public health interventions and behaviors.
By providing a comprehensive and authoritative assessment of the current state of knowledge on vaping, a surgeon general’s report has the potential to empower individuals, policymakers, and healthcare professionals with the information needed to make informed decisions and implement evidence-based interventions.
In conclusion, the urgent need for clarity on the topic of vaping is paramount in light of the prevailing misconceptions, conflicting messages, and the lack of long-term evidence.
The release of a surgeon general’s report has the potential to address these challenges by providing a comprehensive and authoritative assessment of the relative risks and benefits of vaping, thereby dispelling confusion and guiding evidence-based public health interventions and policies.
As the public health community grapples with the evolving landscape of vaping, it is imperative to prioritize the generation of robust evidence, the dissemination of accurate information, and the formulation of informed policies to safeguard public health and well-being in the face of emerging challenges.
Cigarette smoking and vaping have been the subjects of extensive public health debates and regulatory interventions in recent decades.
The adverse health effects of smoking are well-documented, with significant efforts made to reduce smoking rates and mitigate its impact on public health.
In contrast, the emergence of electronic cigarettes (e-cigarettes) and vaping has introduced a new dimension to the tobacco control landscape, prompting discussions about their potential benefits and harms.
This essay aims to provide a comprehensive analysis of smoking and vaping, examining their respective health impacts and the evolving public health policies surrounding these practices.
The history of tobacco control in the United States is marked by significant milestones and policy interventions.
The Surgeon General’s report in 1964, which unequivocally linked smoking to adverse health outcomes, served as a catalyst for transformative public health measures.
Subsequent actions, such as warning labels on cigarette packs, advertising bans, and taxation policies, have contributed to a gradual decline in smoking rates over the decades.
These efforts have been instrumental in reducing the prevalence of smoking and raising awareness about its detrimental effects on public health.
The introduction of e-cigarettes as a potential harm reduction tool for smokers has reshaped the tobacco landscape.
Proponents of vaping argue that these devices offer a less harmful alternative to traditional cigarettes, potentially aiding in smoking cessation efforts.
However, the rapid rise in e-cigarette use, particularly among youth, has raised concerns about a new generation becoming addicted to nicotine.
The popularity of vaping among adolescents has prompted public health officials to address the potential risks associated with youth nicotine addiction and its long-term implications.
The contrasting trends in smoking and vaping prevalence underscore the complex interplay between public health policies and evolving consumer behaviors.
While smoking rates have declined significantly since the 1960s, the rise of vaping has presented new challenges for tobacco control efforts.
The debate over the relative safety of e-cigarettes compared to traditional cigarettes has sparked discussions about harm reduction strategies, risk communication, and regulatory frameworks for emerging tobacco products.
The health consequences of smoking are well-documented, with cigarette smoke containing thousands of chemicals, including numerous carcinogens.
In contrast, studies have suggested that the vapor from e-cigarettes contains fewer chemicals and lower concentrations of toxic substances compared to cigarette smoke.
While this has led some experts to advocate for vaping as a safer alternative to smoking, the long-term health effects of e-cigarette use and exposure to vaping aerosols remain areas of ongoing research and concern.
The evolving landscape of smoking and vaping has prompted regulatory responses aimed at balancing harm reduction with youth tobacco prevention.
The Food and Drug Administration (FDA) has taken steps to regulate e-cigarettes and vaping products, including authorization of certain products as potentially less harmful alternatives for adult smokers.
Simultaneously, efforts to curb youth vaping, such as flavor bans and marketing restrictions, have been implemented to address the rise in adolescent e-cigarette use.
In conclusion, the dynamics of smoking and vaping reflect the evolving challenges and opportunities in tobacco control and public health.
While smoking rates have declined over the past decades, the emergence of e-cigarettes and vaping has introduced new complexities to the tobacco landscape.
As public health officials navigate the risks and benefits of vaping, it is essential to continue research efforts, monitor trends in tobacco use, and implement evidence-based policies to address the evolving patterns of nicotine consumption.
Ultimately, a comprehensive approach that considers the health impacts of both smoking and vaping, while addressing the needs of diverse populations, is crucial for advancing public health goals in the context of tobacco control.
The topic of vaping and its potential dangers to non-smokers is a complex and multifaceted issue that demands careful consideration.
As the use of electronic cigarettes continues to grow, concerns about their impact on public health, particularly among young people, have become increasingly prominent.
The debate surrounding vaping encompasses a wide range of factors, from the physiological effects of nicotine to the regulatory landscape and the societal implications of its popularity.
Dr. Neal Benowitz, a prominent voice in the field of nicotine and tobacco addiction at the University of California, San Francisco, has highlighted the diverse array of studies on vaping, noting that the findings are often inconclusive and varied.
This lack of consensus is further compounded by the challenges in isolating the effects of vaping from those of previous cigarette smoking, making it difficult to draw definitive conclusions about its health implications.
Several studies have indicated potential adverse effects of vaping on respiratory health, particularly in young individuals, with reports of bronchitis symptoms and exacerbation of asthma.
Furthermore, research suggests that vaping may impact the cardiovascular system, potentially leading to concerns about heart disease.
The addictive nature of nicotine, a primary component of both traditional cigarettes and e-cigarettes, remains a significant area of concern, with potential implications for brain development and mental health, particularly among adolescents.
In light of these findings, questions about the efficacy of vaping as a smoking cessation tool have arisen, with conflicting results from various studies further complicating the issue.
The World Health Organization has raised alarms about the proliferation of e-cigarettes, particularly their appeal to young people through a wide array of flavors.
These concerns have prompted calls for regulatory measures to curb the use of e-cigarettes among children and young adults.
The U.S. Surgeon General has also underscored the potential risks associated with nicotine use in any form for young individuals, emphasizing the need for preventive measures.
The regulatory landscape surrounding e-cigarettes has been the subject of debate, with the FDA’s efforts to oversee and regulate these products drawing both support and criticism.
The proliferation of diverse e-cigarette devices, coupled with the emergence of flavored disposable products, has contributed to the complexity of the regulatory challenge.
Despite the growing popularity of e-cigarettes, recent data indicates a decline in vaping among high school students, albeit with uncertainties about the factors driving this trend.
The 2019 outbreak of vaping-related hospitalizations and deaths linked to THC-containing products has further intensified public concerns about the safety of e-cigarettes.
This has prompted calls for more comprehensive studies to better understand the potential health risks associated with vaping.
Amid these discussions, it is essential to recognize the broader societal context in which vaping occurs. Sherri Mayfield, a postal worker, reflects on the public perception of vaping, particularly in light of the 2019 outbreak, underscoring the need for further research to inform public understanding and policy decisions.

The broader implications of vaping, including its potential impact on public health and the need for concerted efforts to address youth vaping, have been highlighted by the surgeon general’s office.
In conclusion, the issue of vaping and its potential dangers to non-smokers remains a topic of significant concern, requiring a nuanced and comprehensive approach.
The diverse array of studies, regulatory challenges, and societal implications underscore the complexity of this issue.
As we navigate this landscape, it is imperative to prioritize further research, regulatory measures, and public awareness efforts to address the potential risks associated with vaping, particularly among young individuals.
Only through a concerted and collaborative approach can we effectively address the multifaceted challenges posed by the increasing prevalence of e-cigarettes in our society.