The recent development in the field of organ transplantation has brought about a new ray of hope for patients suffering from liver failure.
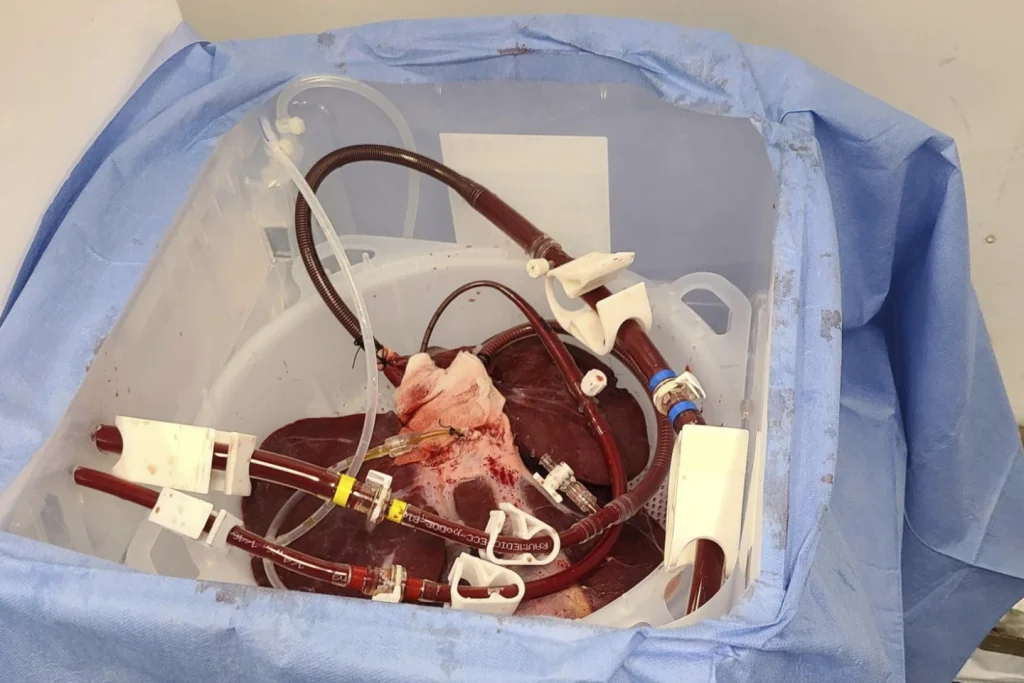
Surgeons at the University of Pennsylvania have conducted a groundbreaking experiment, wherein they externally attached a pig liver to a brain-dead human body and observed its successful filtration of blood.
This significant achievement marks a crucial step towards potentially using this technique in patients with liver failure, offering a glimmer of hope for those in need of life-saving organ transplants.
The experiment, which was announced by the University of Pennsylvania, represents a unique approach to animal-to-human organ transplants.
Unlike traditional methods, wherein the transplanted organ is placed inside the recipient’s body, the pig liver in this case was utilized externally, serving as a “bridge” to support failing livers by conducting the organ’s blood-cleansing function outside the body.
This approach is akin to the concept of dialysis for failing kidneys, thereby presenting a novel and promising avenue for addressing liver failure.
Historically, animal-to-human transplants, also known as xenotransplants, have faced significant challenges, primarily due to the rejection of foreign tissue by the recipient’s immune system.
However, with the advancement of genetic modification technology, scientists have made significant strides in this area.
Pigs, whose organs have been genetically modified to closely resemble human tissue, are now being considered as potential sources for organ transplantation.
In recent years, there have been notable advancements in the field of xenotransplantation. Kidneys from genetically modified pigs have been temporarily transplanted into brain-dead donors to evaluate their functionality, yielding promising results.
Additionally, there have been instances where heart transplants from pigs were performed on human recipients, albeit with limited success.
The successful external attachment of a pig liver to a brain-dead human body represents a significant breakthrough in the quest to address the pressing need for organ transplants.
This pioneering approach offers a glimmer of hope for patients suffering from liver failure, providing a potential lifeline for those awaiting life-saving organ transplants.
The implications of this achievement extend beyond the realm of medical science, offering a renewed sense of optimism for individuals grappling with the challenges of organ failure.
The potential for utilizing genetically modified pig organs as a viable source for transplantation could revolutionize the field of organ transplantation, offering a sustainable solution to the perennial shortage of human donor organs.
While the success of this experimental procedure is indeed a cause for celebration, it is important to exercise caution and diligence in further research and clinical trials.
The ethical, medical, and logistical considerations surrounding xenotransplantation necessitate thorough evaluation and careful deliberation to ensure the safety and efficacy of these novel procedures.
In conclusion, the successful external attachment of a pig liver to a brain-dead human body represents a significant milestone in the field of organ transplantation.
This achievement holds the promise of offering a viable solution for patients with liver failure, ushering in a new era of hope and possibility in the realm of medical science.
As researchers continue to explore the potential of xenotransplantation, it is imperative to approach these advancements with a balanced perspective, mindful of the ethical and practical implications, while remaining steadfast in our commitment to advancing medical innovation for the betterment of humanity.
The U.S. Food and Drug Administration (FDA) is currently deliberating on whether to permit a select group of individuals in dire need of organ transplants to participate in rigorous studies involving the use of pig organs, specifically hearts, kidneys, and potentially livers.
This consideration has sparked widespread debate and discussion among medical professionals, bioethicists, and the general public.
The potential for using xenotransplantation to alleviate the growing organ shortage is both promising and contentious, raising critical questions about medical ethics, safety, and the future of organ transplantation.
This essay aims to provide a comprehensive analysis of the ethical, medical, and societal implications surrounding the use of pig organs for transplantation, focusing on the complexities of liver transplants and the recent advancements in xenotransplantation research.
The shortage of human organs for transplantation has reached a critical level, with thousands of individuals on waiting lists for life-saving procedures.
The demand for organs far exceeds the available supply, leading to prolonged suffering and, in many cases, premature death for those awaiting transplants.
The situation has prompted researchers to explore alternative sources of organs, including xenotransplantation, as a potential solution to address the scarcity of suitable donor organs.
In the United States alone, approximately 10,000 individuals are currently awaiting liver transplants, highlighting the urgent need for innovative approaches to expand the donor pool and save lives.
Xenotransplantation involves the transplantation of organs or tissues from one species to another, with pigs emerging as the primary candidates for providing organs suitable for human transplantation.
The genetic modification of pigs, such as those developed by eGenesis, has paved the way for potentially compatible pig organs, offering hope for individuals on transplant waiting lists.
The prospect of utilizing pig hearts, kidneys, and livers to address the organ shortage presents both opportunities and challenges, necessitating a thorough examination of the ethical and medical considerations associated with xenotransplantation.
The ethical implications of xenotransplantation are multifaceted and demand careful scrutiny. Central to this discussion are concerns regarding animal welfare, informed consent, and the potential risks of transmitting infectious diseases from pigs to humans.
The use of genetically modified pigs for organ donation raises ethical questions about the treatment of animals and the ethical boundaries of manipulating animal biology for human benefit.
Moreover, the process of obtaining consent from individuals in need of organ transplants to participate in experimental studies involving pig organs raises complex ethical dilemmas, particularly considering the inherent risks and uncertainties associated with xenotransplantation.
The recent experimental studies, such as the Penn experiment involving the attachment of a pig liver to a preservation device, underscore the remarkable advancements in xenotransplantation research.
However, alongside these advancements, there exist significant safety concerns related to the potential transmission of zoonotic diseases, rejection of pig organs by the human immune system, and the long-term viability of xenotransplanted organs.
The FDA’s deliberation on permitting individuals to volunteer for rigorous studies involving pig organs necessitates a comprehensive evaluation of the safety and efficacy of xenotransplantation, ensuring that the potential benefits outweigh the associated risks for both the individuals receiving the transplants and the broader public health.
The widespread implementation of xenotransplantation would undoubtedly have far-reaching societal implications, influencing public attitudes towards organ donation, animal research, and the boundaries of medical innovation.
Furthermore, the development of a robust regulatory framework is imperative to govern the ethical, legal, and scientific aspects of xenotransplantation, ensuring that rigorous standards are upheld to protect the welfare of both human recipients and donor animals.
The FDA’s decision regarding the allowance of voluntary participation in experimental studies involving pig organs will significantly shape the trajectory of xenotransplantation research and its integration into clinical practice.
The consideration of utilizing pig organs for transplantation represents a pivotal juncture in the field of organ transplantation, necessitating a balanced and comprehensive approach to address the ethical, medical, and societal implications.
The potential to alleviate the organ shortage crisis through xenotransplantation offers hope for individuals in need of life-saving procedures, while simultaneously raising critical questions about safety, consent, and the ethical treatment of animals.
As the FDA deliberates on this complex issue, it is imperative to engage in informed and inclusive discussions that consider the perspectives of medical professionals, bioethicists, patients, and the broader public.
The ethical and medical complexities surrounding the use of pig organs for transplantation underscore the need for a thoughtful and evidence-based approach to navigate the challenges and opportunities presented by xenotransplantation.
The field of medical science has seen remarkable advancements in the treatment of liver failure, particularly in the development of liver dialysis-like machines.
Recent breakthroughs in xenotransplantation research have paved the way for innovative approaches to address this critical health issue.
A notable experiment conducted last month involved the filtration of blood through a pig liver-device for an extended period of 72 hours.
The results were promising, as the donor’s body remained stable, and the pig liver exhibited no signs of damage.
This essay seeks to delve into the significance of this experiment and the potential implications of utilizing pig liver devices in the treatment of liver failure.
The quest to develop liver dialysis-like machines has been a focal point in the medical community for several years.
Early experiments using pig livers were conducted before the advent of today’s more advanced genetic techniques.
Dr. Parsia Vagefi of UT Southwestern Medical Center, an expert closely monitoring xenotransplantation research, highlighted the substantial efforts invested in the development of liver dialysis-like machines.
Dr. Vagefi commended the recent experiment, acknowledging it as a significant stride forward in the pursuit of enhanced care for liver failure.
The combination of pig liver and the innovative device represents a compelling approach that holds promise for the future of liver failure treatment.
Xenotransplantation, the process of transplanting organs or cells from one species to another, has emerged as a potential solution to address the shortage of human organs for transplantation.
The utilization of pig organs, particularly pig livers, in xenotransplantation research has gained momentum due to the physiological similarities between pig and human organs.
The recent experiment involving the filtration of blood through a pig liver-device for an extended duration underscores the potential of xenotransplantation in revolutionizing liver failure treatment.
The stability of the donor’s body and the absence of damage to the pig liver signify a significant step forward in the exploration of pig liver devices as a viable treatment option for liver failure.
The successful filtration of blood through the pig liver-device for 72 hours presents promising implications for the treatment of liver failure.
The ability to maintain the stability of the donor’s body while preserving the integrity of the pig liver demonstrates the potential of pig liver devices in providing effective support to patients with liver failure.
As Dr. Vagefi aptly noted, the combination pig-device approach represents an intriguing advancement in the ongoing efforts to enhance care for individuals suffering from liver failure.
The implications of this experiment extend beyond the laboratory, offering hope for the development of innovative treatment modalities that could significantly improve the prognosis for patients with liver failure.
Despite the promising results of the recent experiment, several challenges and ethical considerations remain in the utilization of pig liver devices for liver failure treatment.
The potential for immune rejection and the risk of zoonotic infections are critical factors that necessitate thorough evaluation and mitigation.
Additionally, the ethical implications of utilizing animal organs for human transplantation warrant careful deliberation.
Addressing these challenges will be imperative in advancing the field of xenotransplantation and harnessing the potential of pig liver devices for clinical applications.
The experiment involving the filtration of blood through a pig liver-device for an extended period represents a significant milestone in the pursuit of innovative solutions for liver failure treatment.
The stability of the donor’s body and the absence of damage to the pig liver attest to the potential of pig liver devices in providing effective support for individuals with liver failure.
As the field of xenotransplantation continues to evolve, the development and utilization of pig liver devices hold promise for revolutionizing the landscape of liver failure treatment.
While challenges and ethical considerations persist, the recent experiment serves as a testament to the remarkable progress in the quest to enhance care for individuals suffering from liver failure.
