In the realm of healthcare, the intersection of medical necessity and insurance coverage often becomes a battleground for patients in dire need. The poignant story of Grace Armant, an 84-year-old battling Lou Gehrig’s disease, sheds light on the challenges faced by individuals seeking access to essential medical equipment.
Despite her inability to speak, Armant’s voice resounds through her struggles with UnitedHealthcare’s denial of coverage for a vital breathing machine, a lifeline in her fight against the debilitating illness.
The narrative of Armant’s ordeal echoes a broader issue faced by patients across the country, where insurers, including UnitedHealthcare, have erected barriers to obtaining crucial home ventilators for individuals grappling with respiratory conditions.
Physicians and healthcare providers decry the arduous process imposed by insurers, forcing patients to navigate through inadequate alternatives before securing approval for the necessary devices.
The reluctance of insurers to cover essential medical equipment, such as ventilators, raises ethical questions about the prioritization of cost over patient well-being.
The surge in demand for home ventilators, as evidenced by the exponential increase in Medicare spending on these devices, underscores the growing need for comprehensive coverage and access to life-saving equipment.
The intricate dance between insurers, healthcare providers, and patients underscores the complex web of regulations, guidelines, and financial considerations that dictate the availability of critical medical resources.
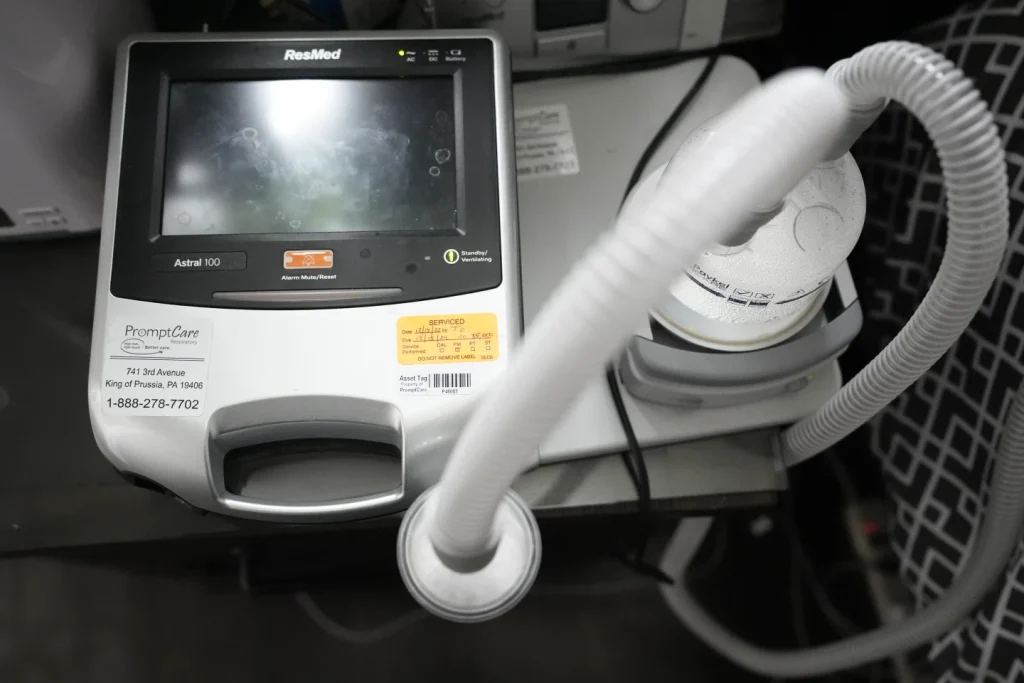
The distinction between noninvasive ventilators and traditional hospital-based devices underscores the evolving landscape of respiratory care, with a shift towards more patient-centric and cost-effective solutions.
The technological advancements embedded in these devices, from battery backups to enhanced functionality, highlight the potential for improved patient outcomes and quality of life for individuals battling chronic respiratory conditions.
The testimonies of healthcare professionals, such as Chuck Coolidge of VieMed, underscore the systemic challenges faced by patients seeking approval for ventilators, both in initial assessments and subsequent reauthorizations.

The apparent uptick in insurance rejections for patients with conditions like Lou Gehrig’s disease and chronic obstructive pulmonary disease raises concerns about the adequacy of current insurance protocols in meeting the evolving healthcare needs of a diverse patient population.
The response from UnitedHealthcare, citing considerations such as patient condition, health plan terms, and Medicare guidelines, underscores the delicate balance between fiscal responsibility and patient care.
The discretionary power wielded by insurers in approving or denying ventilator requests underscores the need for greater transparency, accountability, and patient advocacy in the realm of healthcare coverage.
In conclusion, the narrative of Grace Armant serves as a poignant reminder of the challenges faced by individuals navigating the complex terrain of insurance coverage for life-saving medical equipment.
The broader implications of insurance denials for ventilators underscore the urgent need for a comprehensive reevaluation of insurance practices to ensure equitable access to essential healthcare resources for all individuals in need.
As we reflect on Armant’s plight, let us advocate for a healthcare system that prioritizes patient well-being and dignity above all else.
In the heart of West Virginia, a poignant tale unfolds, shedding light on the arduous journey faced by families navigating the intricacies of healthcare coverage for life-saving equipment.
Dale Harper’s impassioned plea to UnitedHealthcare for his son, Jacob, who battles a rare and aggressive form of ALS, serves as a stark reminder of the challenges individuals encounter in accessing essential medical devices.
The narrative of Harper’s relentless pursuit for ventilator coverage unveils a distressing reality: the bureaucratic hurdles and administrative complexities that often hinder timely access to vital healthcare resources.
Despite the urgency of Jacob’s condition, it took months of appeals and a heartfelt appeal before the insurance provider relented, underscoring the profound impact of insurance company policies on the lives of vulnerable patients.
The poignant accounts of individuals like Armant, residing outside New Orleans, further underscore the pervasive nature of ventilator coverage complications.
The ordeal faced by Armant and her family in securing adequate coverage paints a somber picture of the struggles endured by those grappling with debilitating illnesses.
The looming specter of financial constraints adds another layer of complexity, with Armant’s daughter grappling with the daunting task of sourcing a ventilator amidst financial constraints.
The plight of DeMarco, a Temple student, serves as a poignant reminder of the profound impact of insurance company decisions on individuals’ quality of life.
The denial of a second breathing machine by Aetna and the subsequent appeals process unveil the disheartening reality faced by patients reliant on medical technology for their well-being.
DeMarco’s frustration at the intersection of healthcare, insurance, and bureaucracy resonates deeply, highlighting the systemic challenges that impede seamless access to essential medical equipment.
Dr. Lisa Wolfe’s insights into the evolving landscape of ventilator technology shed light on the underlying factors driving coverage complexities.
The surge in ventilator usage for non-life-threatening conditions underscores the shifting dynamics shaping insurance company policies, with insurers grappling to adapt to the evolving healthcare landscape.
The repercussions of these policy shifts are acutely felt by patients like Jacob, Armant, and DeMarco, whose lives hang in the balance of insurance company decisions.
The poignant narrative woven by healthcare professionals like Dr. Hansen-Flaschen underscores the stark consequences of inadequate ventilator coverage.
The harrowing prospect of patients facing premature death due to inaccessible medical equipment serves as a sobering reminder of the profound impact of insurance company policies on human lives.
The revolving door of hospitalizations and limited treatment options faced by ALS patients without ventilator access paints a grim portrait of the stark realities confronting individuals navigating the healthcare system.
In conclusion, the challenges surrounding ventilator coverage serve as a poignant reminder of the intricate interplay between healthcare, insurance, and patient well-being.
The narratives of individuals like Jacob, Armant, and DeMarco underscore the urgent need for systemic reforms to ensure equitable access to essential medical equipment.
As we confront the complexities of healthcare coverage, let us heed these narratives as a call to action to advocate for policies that prioritize patient well-being and ensure that no individual is left to navigate the labyrinth of insurance bureaucracy alone.
