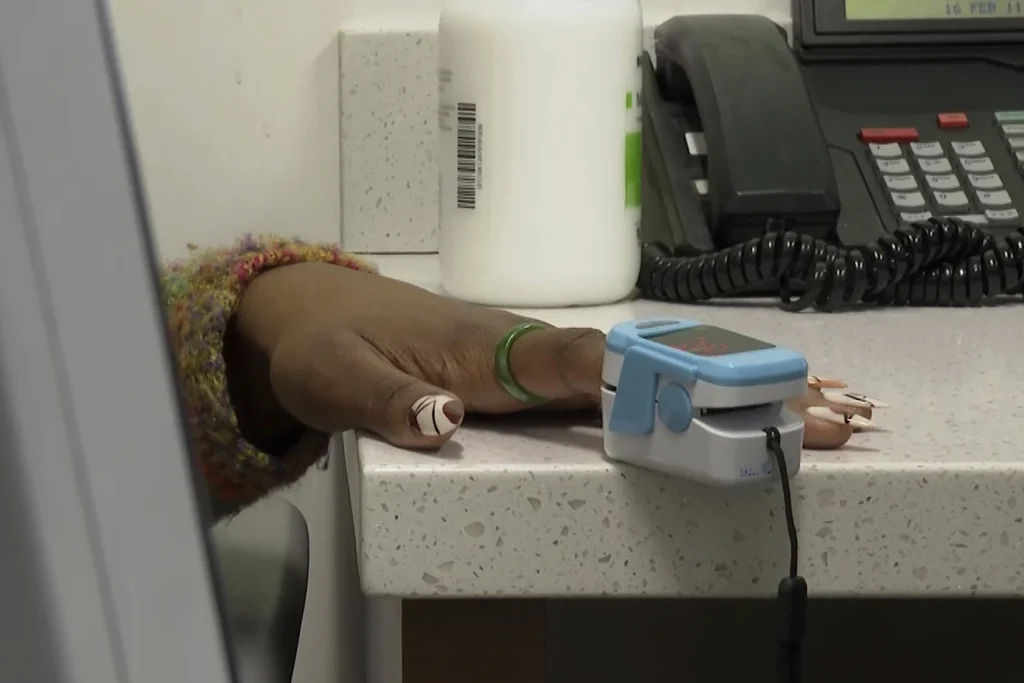
The case of Jazmin Evans, a patient who was unknowingly disadvantaged by a racially biased organ test in the organ transplant system, sheds light on the pervasive issue of racial inequity in healthcare.
This essay delves into the implications of racial biases in medical algorithms, particularly in the context of organ transplants, and advocates for a paradigm shift towards health equity in healthcare practices.
The revelation that Evans should have been placed on the transplant list four years earlier due to the inaccuracies of a race-based kidney function test underscores the systemic racial biases that have long plagued the healthcare system.
The use of a formula that inaccurately assessed the kidney function of Black individuals not only delayed necessary transplants but also exacerbated existing disparities in access to healthcare services.
In response to this alarming discovery, the National Kidney Foundation, American Society of Nephrology, and the U.S. organ transplant network initiated measures to rectify the injustices perpetuated by the race-based organ test.
By recalculating the waiting times of over 14,000 Black kidney transplant candidates and prioritizing those who were adversely affected by the biased test, the transplant network aimed to address the historical injustices faced by Black patients in need of organ transplants.
The case of racially biased medical algorithms extends beyond organ transplantation and highlights a broader issue of racial disparities in healthcare.
Medical algorithms, ranging from treatment guidelines to diagnostic tests, often incorporate race or ethnicity in ways that disadvantage patients of color.
These embedded biases not only perpetuate inequities in healthcare outcomes but also undermine the trust and confidence of marginalized communities in the medical system.
As Dr. Michelle Morse aptly points out, the misuse of race in clinical algorithms has been a longstanding concern among health equity scholars.
To achieve true health equity, it is imperative to dismantle the systemic biases ingrained in medical algorithms and prioritize the development and implementation of race-neutral healthcare practices.
By adopting race-free equations in medical decision-making and ensuring that algorithms do not perpetuate disparities based on race or ethnicity, healthcare providers can strive towards a more just and equitable healthcare system.
The case of Jazmin Evans serves as a poignant reminder of the urgent need to address racial inequities in healthcare, particularly in the realm of organ transplantation.
By acknowledging and rectifying the biases present in medical algorithms, healthcare professionals can take a crucial step towards promoting health equity and ensuring that all patients receive fair and equitable treatment.
It is incumbent upon the healthcare community to confront and dismantle the systemic racism that pervades medical practices, thereby fostering a more inclusive and just healthcare system for all individuals.
In the realm of healthcare, the winds of change are beginning to blow, albeit slowly. Recent developments have seen a shift away from the longstanding practice of incorporating race into medical assessments, particularly in the context of determining health risks and treatment approaches.
This shift marks a significant departure from the traditional norms that have influenced medical decision-making for decades.
One notable example of this shift is the evolving approach in obstetrics, where obstetricians are no longer expected to factor in race when assessing the risk of a pregnant woman attempting vaginal birth after a prior C-section.
Similarly, the American Heart Association has taken a progressive step by eliminating race from a widely used calculator that predicts individuals’ risk of heart disease.
Additionally, the American Thoracic Society has called for the replacement of race-based evaluations in lung function assessments, signaling a broader movement towards more equitable healthcare practices.
The narrative takes a unique turn when we delve into the realm of kidney health, where efforts are being made to rectify past injustices.
The disparity in kidney failure rates between Black Americans and white individuals sheds light on the deep-rooted inequities that persist within the healthcare system.
Statistics reveal that Black Americans are over three times more likely than their white counterparts to experience kidney failure, underscoring the urgent need for reform.
Central to the discussion is the recognition that race is not a biological determinant akin to age, sex, or weight; rather, it is a social construct that has unjustly found its way into medical calculations and assessments.
The case of estimated glomerular filtration rate (eGFR) serves as a poignant example of how historical misconceptions about creatinine levels led to the inclusion of race-based adjustments in kidney function evaluations.
This practice, which could overestimate kidney function in Black patients by a significant margin, has perpetuated disparities in healthcare outcomes.
The process of dismantling these ingrained biases is not without its challenges. The journey to rectify past wrongs often involves painstaking efforts to unearth historical records, recalibrate assessments, and ensure that all patients receive fair and equitable treatment.
Transplant centers have had to embark on investigative missions, scouring through archives and collaborating with healthcare providers to rectify past oversights and ensure that patients receive the care they deserve.
The story of individuals like Evans, who navigated the complexities of kidney disease and transplantation, serves as a poignant reminder of the human impact of these systemic biases.
Evans’ journey, marked by years of dialysis and waiting, underscores the profound implications of delayed interventions and the importance of timely and equitable healthcare practices.
As the healthcare landscape continues to evolve, it is imperative that we remain vigilant in our efforts to address and rectify racial biases in medical practice.

By acknowledging past injustices, implementing policy changes, and prioritizing equity and equality in healthcare delivery, we can pave the way for a more just and inclusive healthcare system.
In conclusion, the narrative of change in healthcare is unfolding, bringing to light the imperative of dismantling racial biases and fostering a more equitable and compassionate healthcare environment.
Through collective action, policy reforms, and a commitment to rectifying past wrongs, we can forge a path towards a healthcare system that upholds the principles of equity, fairness, and dignity for all.
